Hi,
I am a type II diabetic whose pharmacy(Rite Aid) is closing. For the last 3 years I have been getting insulin for my Medtronic insulin pump from them at no cost. I have original Medicare and a supplement G plan. The small amount Medicare doesn’t pay, about $60, gets paid by United Health Care, G plan. I went to the new pharmacy where my scrip was transferred to and I asked the pharmacy NOT to bill this thru my prescription drug plan, but to bill it under Part B, durable medical equipment under Medicare. They told me the scrip would cost $105.00. I mentioned that because I wear an external insulin pump, the insulin supplied for that pump comes with it at no charge. Then they asked me to contact United Health Care and get the RXBin,RXPCN and RXGroup numbers. I called UHC and they told me that they do not have numbers like that. They said just tell them to bill under DME, part B. I went back and told the pharmacy that and they pretty much told me I am out of luck unless I can get those numbers to them. Can anyone out there offer any guidance as to how they get their insulin paid for and not charged?
Thank you,
Stay healthy out there:)
Not all pharmacies can bill Medicare Part B. CVS and Walgreens can, others like Rite-Aid and grocery pharmacies subcontract the work out to Advanced Diabetes Supply. While the companies can bill Part B, finding a pharmacy staffed with people who know how to do it, as you found, can be tough. You might need to visit multiple pharmacies around you to find one with good staff.
Last time this came up CVS inside Target was recommended because they are less busy. A regular CVS should work. Walgreens is a pharmacy of last resort because they are also going out of business. If you are using Humalog or Lispro there are some DME mail order companies that can also supply your insulin. Here’s a topic from last year the covers everything about Part B paying for insulin
This is very helpful info. Thank you for taking the time to respond to me. I will try and contact Afvanced Diabetes Supply tomorrow.
I had to move my CGM order to ADS and was on the phone with them yet again today about it. They got bought by the company that owns Edgepark last year and ADS is now exactly like Edgepark.
Thanks for the info. I know it’s frustrating to get the supplies u need to live with when u need them. Feel ur pain…
I’ve been doing mine through Walgreens and it took like 6-8 weeks to finally figure it out after starting on Medicare. The logjam broke when we figured out it had to be cleared through the Walgreens Medicare Benefits manager or some such job title. Smooth sailing since then. I don’t know from other drug stores but presumably the ones that can do it have something similar.
I know Walgreens has been having financial problems and has been closing some individual pharmacies, including a number in my area. My understanding is that it’s at least partly being done in areas of “market saturation”—like 3 Walgreens in a town that also has a CVS or two, kinda thing. My local one is actually the only pharmacy in town and I was given to understand it’s not under the axe. But who knows. Really don’t want to go through the whole Insulin-as-DME obstacle course again with a whole new supplier. Appreciate the info, though, if it becomes necessary.
I had to jump hoops for about 3
Months at Rite Aid until they could figure out how to help get my orders through. I still have some difficulty at times, but the pharmacist knows me now, and does their best to get my insulin. Sometimes I get 1 month supply and sometimes I get a 3 months supply while my scrip indicates 3 months always. No cost as I have original Medicare with a supplement plan. I consistently have to go to the pharmacy at least 2 times for every order. Finding the right individual who is willing to go the extra mile to help you is hard. Persistence pays off also. I have learned quite a bit through this process.
Thanks for your feedback.
Hi,
I have original Medicare and a supplement through UHC. I have not been paying for my insulin for probably the last 3 years. They should run everything through Part B, DME, and not do anything with the Part D drug plan
from my experience. The pharmacy always seems to try and bill it under the Part D, drug plan, which is incorrect from what I have experienced. Be persistent and find the right person who is willing to investigate things for u.
So, they aren’t going out of biz. They were bought by private equity. That’s why we say a real rough patch with Walgreens. They have closed a number of stores.
Mine have stabilized. They were intentionally running them short staffed for a good long while. If your specific Walgreens is still open, I would expect it to have stabilized by now.
CVS stores are turning into a bunch of Dollar Generals.
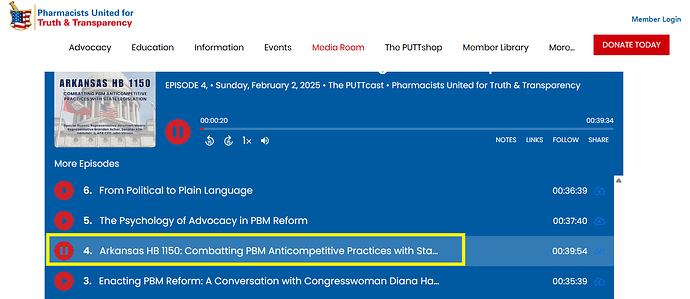
A couple states just broke the pharmacy leg off of the PBMs. You will see a lot more of this (at a state level) in the upcoming session. If you are curious about this, you can learn more here:
I am on Medicare, with UHC plan G. My insulin (lispro) gets billed through Medicare part B DME. I get insulin for 3 months at a time, paying $105. Usually I meet my deductible for prescriptions by May, and after that my insulin is free.
Mike
They might be trying to bill your Part D or they might be billing Part B and failing to bill your Part G plan as secondary. What pharmacy are you trying to purchase from? Sometimes I can find the instructions for what they should be doing in their particular system.
I am ordering from Giant Eagle Pharmacy.
Thanks
Mike,
UHC, my supplemental insurance, had been picking up the total balance for my Insulin over the last 3 years. Whatever Medicare didn’t pay, United Health Care has picked it up. I think there is a problem with how our insulin gets billed by these pharmacies. There needs to be an easier process for those that wear insulin pumps to get their supplies for the pump every 3 months and their insulin.
Retail pharmacies and their mail order services should all be able to handle the general public’s needs for their insulin as this is who most of us go to first to purchase our meds. Just my opinion.
I tried and failed to find a specific answer. They use software called EnterpriseRx. I couldn’t find if they enter your Part G plan on the third party or coordination of benefits screen.
if I were you I’d verify they were billing Part B (B as in bless your heart) and not Part D (D as in don’t you dare). Verify they can bill insulin to Part B.
If they are billing Part B then start with asking them to look up how to add your Part G as a secondary payer. If no luck or a blank look ask for a manager or pharmacist. Last thing would be to ask them to call their pharmacy helpdesk while you wait.
Thank you,
I will verify that.
Not sure this is a good idea, but you could report as fraud for billing part D as fraud. Other thing about Part B and insulin used in pumps is that a pharmacy may not be approved/participating in Part B and so unable to bill as DME.
I am in Akron, Oh area, using Giant Eagle Pharmacy also. A few years ago, the first time got my Insulin for my pump from them, took weeks to get them to process it through Medicare part B. Many at the pharmacy were not aware how to do it properly. I just kept calling and escalating, eventually they got it done properly. There is a special form they have to submit.
I had called Medicare, and had to talk to several people before I got one that was even aware of the special Part B Insulin coverage for Pumpers. I have supplemental G through Medical Mutual of Ohio, Medicare covers the 80%, the supplemental covers the 20%, I pay NO copay.
I also have a Part D plan, and they process that ok, sometimes I use GoodRx for lowest price.
That is too bad. I have used ADS for a couple of years now and have always been very pleased with their service. I hope that does not change
Oops…
I have used ADS for a couple of years now and have liked their service. Hope it does not change now
Good to know. Thank you so much for the information.