Okay, I’ve waited half an hour to recover from this low and no go yet, so I’m just going to go ahead and post…
This is a pretty average day-in-the-life-of-Type-1-diabetes for me. It sums up pretty well what I struggle with much of the time.
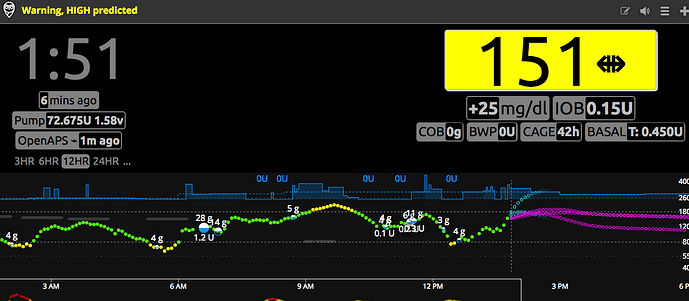
Three days ago I was running high literally non-stop—Thursday I spent 84% of my time high, Friday I spent 86% of my time high. So over the weekend I raised my basal rates and ratios gradually, and on both days I spent 50% and 46% of my day high, respectively, but knowing how these things go (and that I suspect I have increased insulin resistance when I’m high), I lowered my basal rates by 0.05 units an hour and left things as they were.
So, last night I bolused for a granola bar before bed because I was starving (I don’t typically eat right before bed unless I’m treating a low), and then went low at midnight. I treated with six glucose tablets (24 grams of carbs). I came back up but had a pretty sharp drop betwen 4:00 and 6:00 AM. That happens to correspond with the start of my DP coverage, and I noticed I had a drop on Sunday morning, too (I actually woke up low and then had another low, hence why I lowered things by 0.05 units an hour). So, I lowered the segment that runs from 4:00 to 10:00 AM by 0.1 units an hour. I bolused for 10 grams of carbs for my breakfast of scrambled eggs, sausage, almond milk, and almond bread and peanut butter. Seemed to be flatlining.
I had a meeting during the morning. I couldn’t eat most of what was there as it was all wheat-based stuff. But they did have a bowl of grapes, so I took a bunch of grapes and bolused for 15 grams of carbs. (I didn’t look them up and I didn’t weigh them. But I later checked and, according to Google, a cup of grapes is 17 grams of carbs.) At some point after eating them I looked at my CGM and saw that I was rising quite sharply (but not yet high), so I corrected the high. About half an hour later the CGM alarmed that I’d gone crossed my high threshold and there was now a straight up arrow. So I corrected the high again (taking into account IOB). Half an hour later I checked again to find that I’d spiked WAY beyond what I should hav spiked even if I had skipped bolusing for the grapes all together. This is the type of thing that, for me, can easily lead to all day spent high if I’m too passive about it. So, I decided to do a full correction bolus, ignoring all the IOB on my pump. This is a sure way to get a high down fast, but in hindsight I likely ended up stacking insulin on its tail end (my DIA is set to 4.5 hours). I did said bolus at 11:00. Ate lunch at 1:00, which consisted of a soy latte and a granola bar (not healthy, I know, but I forgot a proper lunch and there’s nowhere to stop to grab anything that I can eat). I debated not bolusing for that food at all, but it was 45 grams of carbs, and given what happened with those grapes, I decided to bolus for the whole thing. But, knowing that I tend to go low in the afternoon, I did decrease my insulin to carb ratio slightly.
At 2:00 the alarm I have set on my pump to remind me to try to deal with the lows I always get while commuting home from work went off. I’ve been decreasing my basal segment for that time of day, but no matter what my blood sugar is like, I always go low during that commute home. Even on Thursday and Friday, when 84-86% of my readings were high, I dipped low (on Thursday quite low) during that period. Yet, on weekends I’ve fasted through from breakfast until dinner and, without the commute, I do NOT go low, so I’m reluctant to fiddle with my basal rates too much. Right now, my strategy is to do a -50% basal rate on my pump for two and a half hours starting at 2:00. So this is what I did. Around 3:00 I noticed that I was going down, so I ate a small apple and about four glucose tablets (about 26 grams of carbs). Was on a conference call as I left work, and on the way home went low again and age six glucose tablets (24 grams of carbs), because I was wanting to go get a haircut and did NOT want to go low while I was in the hairdresser chair (but I made sure my Dexcom and glucose tablets were in my pocket, not in my bag, just in case).
Picked up some groceries and came home and posted this. Ate several more glucose tablets on the way home, maybe four. Got home and ate a few more. Proceeded to drop to LOW. Reduced all basal rates on my pump by 0.15 units an hour. Also reduced all my I:C ratios by two, except for the one in the morning, which I left as-is.
And that’s about where I am now. Dinner will be spaghetti squash and chicken, hopefully low-carb enough that it won’t mess things up too much. Unless I keep going low (and I’m still low as I type this), I’ll try to keep my pump settings the same for the next day or two to see what happens. I think my multiple lows this afternoon despite so many carbs (about 74 grams of carbs) is due to stacking insulin: I probably could have reduced my bolus at 1:00 by significantly more, but given that the lows have continued on more than seven hours after that bolus, my basal is probably too high as well. I think that, most likely, these huge fluctuations are due to hormones. But, I can never be totally sure. It’s a never-ending saga for me. I do basal tests that seem to work perfectly one week, and within a week or two my control has totally changed once again. At least for today I’ve spent 68% of my time in range. But the lows are definitely a problem. Three days ago the highs were definitely a problem. There is no easy balance in the middle, at least not that I’ve been able to find over 25 years, but I keep trying and on occasion I do get the balance right and have a glorious flatline day.



 .
.