So, we’re on our 3rd successful POD now and we feel that his sugars are coming under control…even if just a little! We’ll take what we can get. We are seeing many more “level” areas…or relatively level, for sometimes 8 to 10 hours at a time (mostly when he’s fasting…which makes sense, during the night.)
Our biggest problem right now are post-meal highs. It seems that no matter how we adjust bolus insulin, timing between bolus and meals, extended bolus, etc., the spikes never seem to be remedied.
Our Doctor’s have him on a 1:30 ratio, but we’ve taken that down to 1:24 because the spikes were just astronomical…we’re talking above 400 “High” and staying there for hours. Although the spikes are now getting lower, it’s a little unsettling to “need” so much bolus for a meal, for a 2 year toddler to avoid spiking over 300! We are already giving, now, 1 unit for every 24 carbs, or .5 for every 12 carbs.
We’ve extended bolus over a 1 hour, 1.5, 2 hour, 2.5 and 3 hour period and tested various insulin levels, often times correcting far above what’s recommended…yet we still get this huge spike after meals.
Let me give you today’s example to illustrate. I took pictures of the day’s activities that I’ll be including, with comments. If someone sees something obvious jumping out that we may be doing wrong, we’re always listening for advice!
So, last night his POD was expired at 2330. So, since he doesn’t need insulin during the nights, and since he was an easy 130 during the night, I removed the old POD while he slept (at 0532), and we planned on installing the new pod sometime early morning. As you can see, the new POD was installed and activated on 1017 this morning and the “daytime” basal insulin regimen kicked off of .10u/hr.

Here’s his current basal daily regimen:

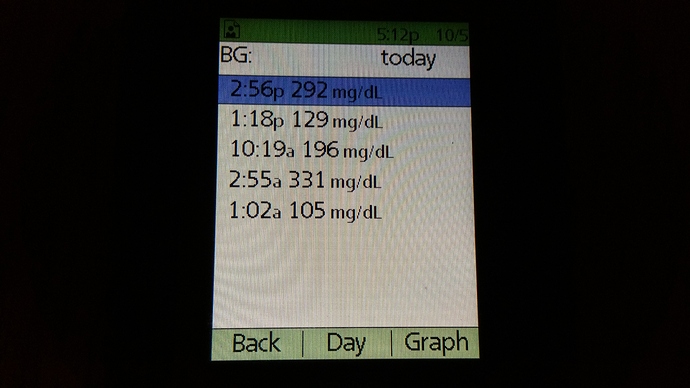
Here’s what his sugars have looked like today so far.:
(as you can see, lots of time “in range”, but two big spikes…AFTER MEALS.
…and here is a zoomed in pic of his most recent spike:
Here is how we bolus’d Liam today so far:

And here are the screens from 10:30AM this morning, through 2:57PM, expanded:
He ate 32g at 1:20PM and was administered 1.3 units of Insulin, which was given at an extended rate of 40% up front and 60% over the next 2 hours.

.10 Units at 14:57 as a correction, even though 0.0 was recommended.

Here are his BG’s from 10:19 this morning (after new pod was installed), to 2:56PM.
Not sure if this is enough information or not…but basically, we’re trying to figure out why such spikes when we’re trying every combination of things we can do. Yes, we’re pre-bolus’ing, sometimes 15 minutes before, sometimes little or no time before (if the BG is really low.) If BG is really high, we’re “correcting the high” first, then when he’s in range, we bolus for meal. We extend meals over different variations of times. We give just the recommended amount of insulin sometimes and other times we give more…sometimes as much as .2 or .25 more.
I can’t think of anything else I just might be doing wrong here. Like I said, I’m very happy with a majority of the day…it’s just the hours following a meal that are killing his A1C, and spiking him so high.
Any recommendations would be appreciated. And if you need more info, I can provide whatever’s needed.
Thanks!