As we were taught: endocrine pancreas, makes Insulin. Exocrine pancreas (same organ, different functional parts) makes enzymes that assist with digestion. Lipase, breaks down fats, amylase, maybe (can’t entirely recall) proteases for proteins, amylase breaks down starches.
Possibly I wasn’t paying attention, glucagon also from endocrine. But isolated glucagon production deficiency doesn’t appear to be a disease entity?
Yes! And probably more. I heartily believe that addressing only the insulin insufficiency is not enough. And that is why I have all kinds of digestive problems. No one even tests nor addresses other lacks nor misfirings from an impaired pancreas.
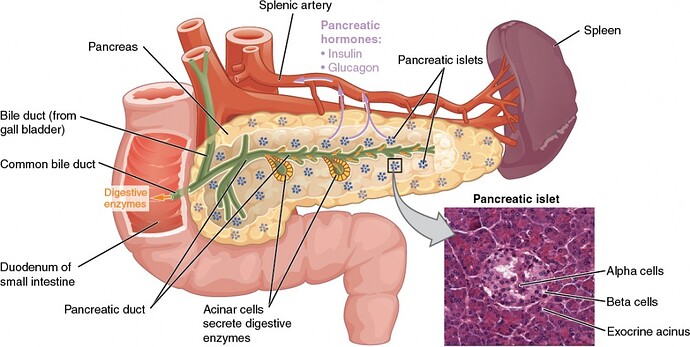
A picture is worth a thousand words, it is said. Here is an image and a couple of snips and links about the functions of the various pancreatic endocrine hormones. These cells make up a very small part of the pancreas with the majority producing digestive enzymes.
- The alpha cell produces the hormone glucagon and makes up approximately 20 percent of each islet. Glucagon plays an important role in blood glucose regulation; low blood glucose levels stimulate its release.
- The beta cell produces the hormone insulin and makes up approximately 75 percent of each islet. Elevated blood glucose levels stimulate the release of insulin.
- The delta cell accounts for four percent of the islet cells and secretes the peptide hormone somatostatin. Recall that somatostatin is also released by the hypothalamus (as GHIH), and the stomach and intestines also secrete it. An inhibiting hormone, pancreatic somatostatin inhibits the release of both glucagon and insulin.
- The PP cell accounts for about one percent of islet cells and secretes the pancreatic polypeptide hormone. It is thought to play a role in appetite, as well as in the regulation of pancreatic exocrine and endocrine secretions. Pancreatic polypeptide released following a meal may reduce further food consumption; however, it is also released in response to fasting.
https://courses.lumenlearning.com/suny-ap2/chapter/the-endocrine-pancreas/
The above leaves out one other hormone secreted by the Beta cells, amylin. Type 1 diabetics will not have this hormone as well as insulin. It is considered not necessary, but that could change.
Amylin is co-stored and co-secreted with insulin by pancreatic islet β-cells. Amylin inhibits food intake, delays gastric emptying, and decreases blood glucose levels, leading to the reduction of body weight. Amylin is co-stored and co-secreted with insulin by pancreatic islet β-cells. Amylin inhibits food intake, delays gastric emptying, and decreases blood glucose levels, leading to the reduction of body weight.
Role and Cytotoxicity of Amylin and Protection of Pancreatic Islet β-Cells from Amylin Cytotoxicity - PMC
@Luis3, thanks so much! This is the very best report I have seen on pancreatic function.
This is true, but it’s the insulin cells that we can’t live without.
The rest we can survive.
People who have their pancreas removed can live with insulin injections.
There is a study being done to convert some alpha cells to beta cells, and I’m hoping that comes to fruition. I assume I have lots of functioning alphas.
Those that have their pancreas removed cannot do without the digestive enzymes. These are necessary to complete the digestion of the 3 macro nutrients- fats, carbs and proteins. Supplements will have to be taken by mouth with each meal, forever.
My father-in-law was diagnosed with pancreatic cancer about 20 years ago. He needed insulin and pills that provided the digestive enzymes.
Our alpha cells are dysfunctional, too. That’s one of the perplexing mysteries we still don’t understand. They’ve discovered hyperplasia of the alpha cells (essentially tumorous-like growth/reproduction of the alphas) in newly diagnosed patients. And they continue to behave inappropriately thereafter, such as releasing MORE glucagon when we eat instead of less.
This paper does a really great job of explaining the broken pancreatic pathways in T1, including glucagon, amylin/amylase, GLP-1, and DPP-4:
View of Alpha cell function in type 1 diabetes | British Journal of Diabetes.
Sorry but I would much prefer that my beta cells are revived and produce insulin again. Research has shown I believe that the other functions are slowly adversely affected over time as well when your beta cells are attacked and you no longer produce insulin. I don’t see the point in denying the reality of the situation. It is what it is.
The paper shows a few examples how alpha cells can be dysfunctional in T1. However, it is important to highlight that the dysfunction does not always result in elevated glucagon levels. The opposite can actually be the case.
Three things must be kept in mind when talking about insulin and glucagon secretion:
- For a long time, islet cells were viewed in isolation. Relatively recently though it has become clear that the islets need to be viewed as a unit because the various types (alpha/beta/etc.) coordinate each other’s function. If beta cells are missing, then the other cells may not function correctly.
- There is a hypothesis that alpha and beta cell activity is also regulated by sensing concentrated secretion of insulin and glucagon. If for example the alpha cell sees a big and very concentrated insulin pulse passing through, its glucagon secretion is suppressed. Since exogenous insulin is infused through the skin and not right inside the islet, the alpha cells don’t see insulin in such high concentrations, and thus their glucagon secretion is not suppressed as much (since the suppression is a function of insulin concentration, not just insulin presence).
- The beta cell destruction seems to sometimes cause collateral damage to other islet cells and also permanent damage to the nerves inside the islets that connect the islet cells to each other. This islet cell neuropathy could further worsen dysregulation of the islet cell activity (since the cells need to communicate to each other).
One outcome can be persistent hyperglucagonemia if the alpha cell glucagon secretion is not suppressed. From what I recall, GLP-1 agonists can help here.
But another possible outcome is that the alpha cell’s response to low blood sugar is blunted. Glucagon is then not elevated as much as it should be. In those cases, people are more prone to experiencing hypoglycemia.
One interesting question is how dysfunctional alpha cells are dealt with if encapsulated islets become available. Are the dysfunctional cells left in? I can’t see how they’d be surgically removed, given how they are distributed in the pancreas.
I’m a big proponent of GLP-1 RAs in T1. I’ve been taking Trulicity for about a year now and it’s absolutely amazing. I feel like it’s fixed things I didn’t know were broken, because the dysfunctional signaling pathways were all I’ve ever known. Suddenly, my body is communicating with itself the way it’s supposed to. The strangest thing for me is the sense of satiety. I never had impulse control with rich and/or sweet foods. Absolutely no sense whatsoever of “oh, that’s just too much, I couldn’t possibly eat another bite…” It was pure self-control to not over-indulge. But now, while I still find things delicious, I can’t stand more than a few bites of them.
I don’t think they’re even being considered at this point. At least not that I’ve read. Are you aware of any research that is producing all the islet cells? I was under the impression they were selecting for just beta cells. I’m pretty sure the crisper-modified proteins that avoid immune detection in the first place method is going to win out over encapsulation techniques, anyway. I do wonder if the portal vein placement is close enough to get any of those symbiotic benefits.
I don’t believe that doctors remember or think about what they were intended to learn in medical school unless forced to do so in everyday practice. Everthing else gets pushed into “someone else’s” problem.
I’ve lost a lot of the faith I once had in the knowledge of medical doctors, while gaining more respect for surgeons. Surgeons must develop personal skill in surgery. Medical doctors in general are poor diagnosticians of anything but very common disorders with easily recognized symptoms.
The paraphrased Physicians Oath is “First, until it’s broken or obviously failing, unless you can fix it, leave it alone”. Implied but not stated is, "When you don’t know what’s happening, say you don’t know what to do. Don’t say there’s nothing to worry about. "
At least surgeons know what things are supposed to look like, pragmatically respond to abnormalities and pretend less to understand exactly how things work at a biochemical level. eg They don’t automatically assume, without knowing other factors, that a broken ankle was a consequence of or associated with diabetes.
Where it breaks down is siloed information. Not every doctor can be as knowledgeable about every condition and disease as multiple specialists, but there’s no excuse for a PCP who refers a patient to a specialist not knowing more than patient about what the specialist tells the patient. There’s never an excuse for a patient to know more than a specialist about nuances and best practices of that specialty or general medicine.
Where surgeons fail is assuming that a person with diabetes is badly self-managing that disease and is a special risk for them, then prescribing medications and special protocols without considering the effects - on good diabetes management.
It’s also my belief that too many doctors think of their customers as one-dimensional, either by a disease or their specialty. Those slapped with the label with “diabetes” (I hate that dysfunctional symptom-based label) are broken glucose consuming machines.
It seems to me that once over 65, I’m increasingly treated as if I was mentally feeble. I now get simplistic explanations that my history and questions already indicate I understand as well as the doctor, and even more simplistic answers, as if I was going to die soon no matter what, so why bother.
I wonder if it’s a coincidence that despite it being the fastest growing demographic, studies of persons over 65 are rarer than those specifically studying any other demographic. I wonder if it’s because we are “unreasonably” well-informed and have “unreasonable” amounts of experience with, and expectations of competence.
The strangest thing for me is the sense of satiety.
Yup, that’s a known effect of GLP-1 agonists, and a very desirable one at that, since they usually are prescribed to type 2 diabetics, which may have a dysfunctional satiety-hunger regulation.
I don’t think they’re even being considered at this point. At least not that I’ve read. Are you aware of any research that is producing all the islet cells?
The Vertex VX-880 trial produced full islets from what I see, not just beta cells. There’s also this.
I’m pretty sure the crisper-modified proteins that avoid immune detection in the first place method is going to win out over encapsulation techniques, anyway.
True, that one is quite promising, and would yield many benefits, since the islets could then potentially live on for longer. From what I recall, maintaining the supply of nutrition to the islets through the encapsulation has been one major problem so far.