I got myself a Pendiq 2.0 electronic pen for the bolus. It is much heavier and longer than my Lantus pen, and setting the dosage is done in an entirely different way, so it is highly unlikely I can ever confuse these two.
As a general rule, I will aggressively defend crossing below 65 mg/dL (3.6 mmol/L) or moving above 140 (7.8). In these situations, I will take into account insulin on board, carbs on board, trends of recent days, change in exercise routine, and things like the nutritional content of a recent meal.
I don’t think bread is capable of causing a late BG spike three hours after eating. The BG effects of bread will usually occur within an hour after eating, if eaten alone. If eaten with protein and fat, the bread carb effects will be delayed.
Unexpected BG spikes 3 hours after eating are often caused by protein and to some extent, fat. If you are eating a carb-limited diet, you will likely benefit from calculating the effect protein will have on glucose and then dosing for it. If you are interested, I can go through the arithmetic involved. It’s not that complicated.
Here’s the thing though. I eat bread very slowly, bit by bit. This can take well over an hour. Sometimes I am not done even 2 hours post-injection. I have to do this to prevent the bread from spiking me too much. I have eaten protein heavy meals in the past, and I didn’t get a spike from it. I’ve read that not everyone gets a protein spike. For some, the spike is very pronounced. For others, it is barely registrable. I do not think honeymoon is responsible for that, since as said, I spike heavily from carbs if I don’t bolus carefully, and I see no reason why honeymoon should help with protein but not with carbs. After all, the residual beta cells don’t distinguish whether the glucose comes from carb absorption or from gluconeogenesis.
If I eat bread relatively quickly, then this won’t happen, yeah. But then the spike will be too high for me. Eating slowly means that I can limit it to maybe 120-130 mg/dL, sometimes even less.
Even eating the bread very slowly cannot explain the spike at 3+ hours post-meal. Do you use a CGM? If you don’t, I think you could learn a lot about your glucose metabolism even with intermittent use.
How do you deliver your insulin? Insulin pump or multiple daily injections. What insulin do you use for your basal, if not on a pump? When do you deliver it, what’s your dose, and if you skip a meal, does your blood glucose remain in a 30 mg/dL (1.7) wide range?
Everyone’s situation is comprised of a variety of factors weighted according to their unique metabolism. Having said that, I believe you can discover how your metabolism works if you keep at it and monitor enough BG data, especially post-meal.
Oh I do have a Libre, combined with a Miaomiao to turn it into a CGM, which is how I discovered that post-meal spike. This is also how I know that protein won’t do that for me. I’ve eaten fish and large amounts of chicken and beef, and the BG curve remained flat.
I use MDI, and use Lantus. I plan on giving Tresiba a try though. Currently I’m at 9 units daily, though this varies. Sometimes I need less, so let’s say 7-9 units. And, if I skip a meal, the BG stays flat. If it rises a little or falls a little, I know I have to adjust the basal.
But to be honest, I am thinking of switching to a pump eventually. I’m waiting for a loop capable patch pump to hit the market, and avoid Medtronic stuff like the plague.
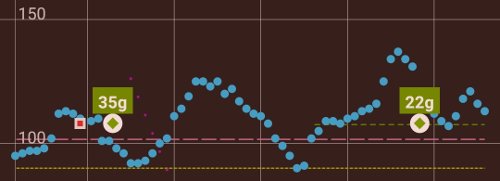
EDIT: Here is the xDrip plot. The 35g were the breakfast. The 22g were lunch. I don’t think a protein spike would be so sudden. It would be much more gradual. To me, it looks as if some carbs were heavily delayed. Remember, I added quite the amount of cheese, ham, and butter.
Those late spikes are a pain! I’ve been seeing more of them since switching to Fiasp, which has a faster onset and shorter “tail.” On the whole I like it, but particularly with meals where there’s a significant amount of fat involved I will get a late spike 3-4 hours after eating because of the delaying effect, and with Fiasp my bolus has pretty well faded out by then. Figuring out how to handle this problem has been tricky. I basically keep an eye on my CGM (I use Sugarmate on my desktop status bar) and as soon as I see that delayed rise start heading up, I’ll bolus a few units to try to stay ahead of it. For me, 140 would definitely not be in the “concern” zone though, after a meal. Actually I’d be pretty happy with it. My problem is that these delayed spikes want to zip right past 160 or so, sometimes into the low 200s.
I agree. That’s not what frustrates me. What frustrates me is that there is this second late spike in the first place. Otherwise, I could just go on with my business after the first peak is done. But with this? I gotta watch the CGM regularly. The worst part is a moment like the one you see when the BG suddenly rose again. There was a slow BG increase, then the second spike. This slow BG increase is the zone where you debate with yourself whether or not to inject. It is maddening.
I am hoping that closed loops can help with catching such unexpected secondary peaks so I can go on with my business. I’m even OK with it spiking a bit as long as the loop takes care of getting it down again.
^^^ I absolutely 100% agree. I hate thinking “Hey, I did pretty good this time!” at 140, two hours after a meal, and then an hour or two later I’m struggling to correct 200 with an up arrow. But it’s so hard to look at that 140 and say “Hey I better take some more insulin!” based on a guess as to what you think might possibly happen a while later. Even an informed guess, like when I know the second spike is likely, based on past experience with a particular meal (like that BLT I treat myself to most Fridays).
We have all these new tools, but the analogy I’ve always used still holds: T1 is like driving a car at speed backwards through town. You’re always swerving back and forth to try and go straight, and you can only tell where you’re going by looking in the rearview.
The reason the honeymoon can handle your protein spike is because it is so slow to turn into glucose whereas bread will turn into glucose very quickly (think a fan on low vs. an air conditioner) even if you are eating it extremely slowly. That technique probably won’t work for very long since your honeymoon will eventually come to an end. If I were you I’d try and figure out how to bolus for the bread so that you can eat at a normal pace unless you like eating for 2 hours.
The spikes are the reason I’ve been avoiding bread for the last year and while I still have to deal with protein spikes I’m at least avoiding going into the 300’s by abstaining from most carby foods.
I am not so sure about that. I have had very slow but consistent BG increases in the past happen to me (unrelated to protein). Honeymoon did not handle them. Also, if the BG is elevated, a strong honeymoon would mean that the beta cells could bring it down slowly. But in my case, it stays elevated. This suggests to me that my beta cells can’t handle mealtime increases anymore (or hardly can), and are probably already completely busy helping out with basal. I’ve also heard of long-time T1Ds who have never had to bolus for protein. I might be one of these people. Time will tell once my honeymoon is over.
That xDrip screenshot helps visualize what you’re up against. I’m thinking your basal insulin, Lantus, is not giving you a good solid platform to launch your meal bolus insulin dose. A fading basal dose causes some of the bolus meal insulin to have to backfill the missing basal.
Small doses, like 9 units, of Lantus are known for not usually lasting 24 hours. Many people who use Lantus split their dose between morning and evening injections. When do you inject your Lantus dose?
I think that second spike could easily be explained as a basal dose fading. Have you observed your BG line when you miss a meal? Does it keep you relatively flat (staying within a 30 mg/dl range)? Have you ever done any basal testing?
Like all the formulas and settings we make with out diabetes technology, it’s not a “set-it and forget-it” tactic. I believe there is no set of perfect insulin settings for anyone. Even the best settings can only put you within reach of your goals. It works best when the formulas enable you to make the final adjustments with micro-boluses micro-carb nudges. Diabetes is dynamic, so if we want to keep BGs reined in, our tactics need to be dynamic as well. If this topic interests you, you may want to read Ponder’s Sugar Surfing. Dynamic diabetes management is one of the themes that runs through his book.
Well, I quote myself from earlier:
I use MDI, and use Lantus. I plan on giving Tresiba a try though. Currently I’m at 9 units daily, though this varies. Sometimes I need less, so let’s say 7-9 units. And, if I skip a meal, the BG stays flat. If it rises a little or falls a little, I know I have to adjust the basal.
All in all, the only thing that adds up is a great carb absorption delay due to the fat and protein.
Agreed on Sugar Surfing though. I’m reading it. Excellent book.
Sorry, I missed this. You have all the tools you need to figure this out. Don’t be afraid to experiment with various things like dose size, pre-bolus time, and even adding a second meal bolus taken after the meal. Good luck.
I experiment all the time  Thanks.
Thanks.
Here’s another question for the veterans - sick days. How do you handle them? I’ve heard the general advice from the endo - drink a lot of water, make sure you eat enough, watch the BG closely, do correction bolus as needed, you may need considerably more (or considerably less) insulin. Try to eat even if you vomit to not risk a hypo. If this isn’t possible, if there’s constant vomiting or diarrhea, go to a doctor, or perhaps call the ambulance (if you bolused and just can’t keep any food down).
In my experience trying to eat when you are vomiting is a bad idea because if you are still sick then it will come back up and if you took insulin for that food then you are in way more danger than if you hadn’t ate and were just running on your basal. As a kid when I was sick I was forced to eat even when sick because of NPH which some people on this forum call eat now or die insulin and they’re right so that would be a reason to keep eating. Modern basal insulins make that advice pretty much obsolete IMO.
Sure, but what if you ate and then started to vomit?
You would most likely need glucagon to counteract the insulin for instance if you had food poisoning.
I’ve been T1 for a long time & I’ve driven myself (& my wife, friends, others) ‘NUTS’ trying to make this disease ‘predictable’… WAY too many ‘factors/variables’ involved despite how much I “OCD” about it. The best you can do…is the best you can do. I ‘try’ my best to utilize my Endocrinologists advice, latest Tech, support from family & friends, and then, I ‘try’ to just accept the results/A1c# & ‘live my life’. Diabetes WILL control your life IF you let it, so I guess my advice is just to ‘Do your best & Enjoy Life’ as much as you can! Hope this is helpful…
Nice to see it’s catching on ![]() Maybe it can just be an acronym: ENOD.
Maybe it can just be an acronym: ENOD.
Back in the NPH days a hospital stay was pretty much required with a stomach virus. Fortunately I only had it happen to me once during that period; unfortunately it was when I was insured through MIT, so it meant a stay in the campus clinic, which was not terrible in itself–it was actually quite decent–but the episode happened to occur in the middle of summer, so I was the only patient in the facility. Sounds great? Not so much. Because the entire nursing staff were bored to tears and only had ME to work on, and boy were they keen on it. Turned me into a total pin cushion. Next day I felt well enough to go home, but they were all about keeping me for another 24 hrs, just for, y’know, observation. 'N stuff. But I totally put my foot down–I’d hardly gotten any sleep while there.
Only other time I had vomiting back then was a case of food poisoning, and fortunately it came on at night when I didn’t have any insulin on board, so I didn’t have to go on an IV and all the rest. Nowadays, with a pump or even basal-bolus MDI I don’t think hospitalization is considered necessary except with little kids or extreme cases, but it was one of the things I was always fearful of on top of the unpleasantness of the sickness itself back in the day. Yet another reason to hate ENOD!
Now that you guys mention NPH, it reminds me of a friend who’s had T1 since 1998. I recently got in contact with him again … he has no CGM, and uses Humalog and Lilly Basal. So, he is using NPH! I told him about newer basals, about upcoming closed loop pumps, about CGMs, he didn’t know anything about these. I was thinking of giving him a Libre starter kit as a birthday present so he can see the light  Because he’s very set in his ways. He also hasn’t seen an endo in years, which perhaps explains why he is still using Lilly Basal - any up to date endo would probably have put him on something else right away.
Because he’s very set in his ways. He also hasn’t seen an endo in years, which perhaps explains why he is still using Lilly Basal - any up to date endo would probably have put him on something else right away.
