I’m a 1.5 and have been injecting a combo of Levemir and Humalog for 6 years. Added Metformin to that mix about two years ago. I also eat a limited carb diet and exercise regularly. I would like to consider switching to a pump, but am wondering if pump users are able to keep their A1C in the low 5 range. I have been able to keep mine at 5.2 for quite a while. I like the forum would appreciate feedback.
Your A1C will be more of a result of what you do rather than how you take your insulin. If you’re able to achieve an A1C that good on shots then a pump shouldn’t change it. If you eat a limited carb diet and have a stable routine a pump may not benefit you that much. In fact, you may find yourself eating more and more carbs since you can just discreetly bolus by pushing a button rather than having to take your syringe or pen out and find a place to do it, and that could push your A1C up!
How do you think a pump would benefit you vs. your current protocol?
Good feedback. I understand. I’m wondering if the perimeters of a pump can be set to be able to maintain blood glucose in the 80’s? I am enticed by the potential to be more spontaneous about eating. For instance, I don’t have insulin with me, should we decide to dine out. I’m also wondering how long insulin is stable in the pump, and if it is outside temperature dependent?
Simply by the ability to be more spontaneous and flexible, whereas now, I always need to plan ahead to have correct insulin dosage with me to eat out.
I never need to plan for any meals and don’t have a restricted diet really, other than excluding obvious things like regular Coke and foods I know from experience will spike me like crazy no matter what I do. I have good control and good A1Cs but I would not be able to maintain blood sugars in the 80s all the time without a significant diet change which I’m not interested in. If you maintain a low-carb diet your blood sugars should be where you want them whether you use pens or pump. The pump is just a dumb computer that does what you tell it. If your goal is better blood sugars than you’re already having I don’t think it will help you. If you want to live life as flexibly as possible, eat as normally as possible, and maintain very good blood sugars while doing this (though not in the 80s all the time) a pump will help you do that. There are other benefits as well (ability to fine-tune basal rates to prevent lows and highs during stress and exercise for example), but a goal of being able to program a pump for perfect blood sugars isn’t realistic. In terms of temperature I refill my pump once a week at most with nearly 300 units and have never had a problem. I know I’m in Canada, but we do get hot summers in Toronto believe it or not and never had an issue!
I target 100, not 80, but otherwise am lower carb and am quite happy with my pump. As you suggested it has given me a much more normal feeling life:
- I never have to skip eating because I didn’t expect to need to bring my pens along.
- It’s much easier to bolus for a big steak with a pump since I can tell it to give me a bit later, and not have to remember to take an extra shot in 2 hours.
- It’s more discrete than pens. My business associates think I’m checking my email on my phone when instead of taking my insulin.
- I can more accurately control my basal, especially for sports. I can get more insulin in the early morning when I need it most and have it totally out of my system in time for tennis at 11am.
After you learn how the pump works, I see no reason why your excellent A1c should change. It will take some time to learn the pump’s operation but you probably already understand insulin to carb ratios, insulin sensitivity factor, and duration of insulin action. The pumps computer will help you with computing meal and correction boluses and will also remember the date and time of these actions. The memory feature alone is valuable to me. When did I take that meal bolus??!
Your interest in tight blood glucose control will likely lead you toward an artificial pancreas system in the years ahead. Starting on a pump now will make you conversant and familiar with pump operation.
One additional feature of a pump is not available with multiple daily injections. Once you deliver your basal insulin on MDI, that’s it – you can’t change it. With a pump however, if you may set a temporary basal rate of say, 0.0 units per hour, for a half hour, in response to a trending low. I think of it it like “taking back” some of my basal dose, a nice feature. Conversely you could set an increased temporary basal rate to help you knock down a trending high.
You obviously know what you’re doing with MDI. The pump does take some learning but it returns that effort with flexibility and it remembers better than most humans. Good luck.
I’ve previously been reluctant to consider a pump because I didn’t think I could maintain as tight of control. This is the 1st forum I’ve participated in. I’m finding all your input very useful before having a conversation with my doctor about a pump. I appreciate the community share of experience!
I should have asked earlier, do you use a continuous glucose monitor? If you don’t, I would rate getting one as delivering more impactful benefits than a pump could in your case. Just a thought…
No, I hadn’t considered that. I manually test 6-8 times daily. I have also been under the impression that manual testing is used in conjunction with a CGM?
It is, with the Dexcom you have to calibrate it by testing every 12 hrs and sometimes more than that. I basically only test when it needs a calibration now though and rely on the CGM throughout the day given how accurate it usually is. I agree with Terry, a CGM is by far the most important device for good control, whether or not you’re on a pump.
I think you can maintain control as good as you have right now on a pump, but it is important to understand the drawbacks too. Sometimes infusion sites don’t work well, sometimes you get air bubbles, and overall basically there will be more variables that you will have to deal with that can, not often, but sometimes, raise your blood sugar temporarily until you fix the problem. I’d say these problems are rare and my control overall is still far better on a pump than it would be on shots. My lifestyle, as others have talked about, is far better on a pump and closer to how “normal” people eat and live. For me, it is important to balance lifestyle and control. I think it’s possible that my control could be better if I ate the same low-carb meals at the same time everyday and took shots, but the slight improvement in numbers would not be worth it to me. If your goal is only about the best numbers possible, you may not see an improvement using a pump and may find it more of a hassle. If your goal is a more normal lifestyle while maintaining very good control that minimizes the risk of long-term complications, but perhaps not necessarily perfect numbers every second of every day, then a pump is for you.
You’re probably aware of the YDMV or “your diabetes may vary” truth most of us recognize here. The best thing about a CGM is that it teaches you about your unique diabetes metabolism. For example, if it were not for my CGM, I would likely not have learned that my blood sugar tends to rise in the morning triggered simply by my “feet hitting the floor” when I get out of bed. Here’s a fairly typical trace this week on my CGM.
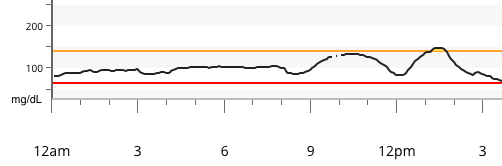
When I woke up around 8:30 a.m., my blood sugar was under 100 mg/dL (5.6 mmol/L). Without eating anything, it rises. The bump between 9 a.m. and noon is not fueled by any food. It would normally rise to the 160-180 (8.9-10.0) range without any counteraction. I take some insulin when I get up, expecting this to happen. In this case I was able to keep the “feet-hit-the-floor” rise to under 140 mg/dL (7.8).
The second BG bump from noon to 3 p.m. is from my late breakfast.
The CGM is a great teacher for those who pay attention. It is an outstanding tool since it feeds your self-knowledge. With diabetes, and most other things in life, knowledge is power.
Yes, Dr. Bernstein "The Diabetes Solution " explains that as "the dawn phenomenon ". I haven’t really looked into CGM devices yet, to know how they work. Do you insert into a different site? Are they sometimes one with a pump?
Current infusion pumps and CGM’s utilize separate sites. That feet-hit-the-floor bump is on top of my dawn phenomena. For me, DP starts at 3 a.m. but the line above benefits from my pump’s basal profile.
Some pumps double as a CGM receiver display but they still have two separate device sites.
Thanks, that makes sense.
There’s been some great responses here from people who get excellent results from pumping.
Like others, the ability to live a more “normal” is key. The temporary basal rate is so great, because life constantly throws curves at me, and the TBR helps tremendously.
Temperature? I lived on a sailboat for five years, much of that in the Caribbean. Last summer, I rode a bike across the USA in the middle of summer. My insulin typically lasts for 9 days before the pump cartridge runs dry. In the 17+ years I’ve been pumping the temperature problems can be counted on one hand.
Does anyone wear a pump into a hot spring or tub or should it be disconnected? I know it’s a different subject, but is there a favorite pump? I’m thin and a little concerned about availability of sites. Somewhere, I read about one of them has the smallest needle, but can’t remember which one. Medtronic sounds interesting because they will provide a 6 week trial. Omnipods aren’t Mac compatible and I’m an Apple user. I don’t know if that’s important or not.
Not sure about this. I connect my Omnipod PDM to my Mac to upload results to Diasend. Omnipod doesn’t currently have any computer interface for controlling the pump, and uploading/viewing your pump data is the only time a computer comes into it.
Omnipods are safe in water (though the PDM isn’t), I believe for up to an hour. I have worn mine in the sauna, for about half an hour. Once this affected the adhesive, but the pump has always worked fine.
