I’ve been at this for so long. I’m loosing my mind. We are all Told if you don’t trust your CGM reading to do a finger stick. Sometimes the finger stick matches and sometimes close. But what concerns me is a major difference and on top of that my main concern with this writing is the multiple difference I get doing finger sticks. I now have to finger stisck 3-4 times and average the reading even though the blood is coming from the same finger. Any advice
Are you using a good meter like a contour one?
I agree with CJ. Start with a good meter like the Contour. Make sure your hands are clean; wash with soap and warm water. Do a second finger-prick if your gut tells you to – I don’t often do this with my trusty Contour Next One.
I rate the finger stick over the CGM reading.
If your glucose variability is low, any food or insulin corrections will be small and low risk. It’s why I minimize total daily insulin and eat low carb.
The problem is that what we want for “close” is always smaller than what we need for close.
Use this to compare your BGM readings to your CGM. Parkes Error Grid | Desmos Its not until your results are landing in zone C that you may need an extra correction or carbs to correct for a dosing decision based on the CGM value. @Yve65 I wanted to share this with you too.
I also agree with CJ on meters and with Terry about rating the BGM over the CGM. I was talking to someone else about meters and came across a Onetouch study they did for the EU. It was a “do the production meters and strips perform in the real world as good as they did in the clinical trial we did to get the meter approved” study. The study showed the meter met the specs but boy howdy was there a lot more variability than in the original clinical trial. So expect 3 fingersticks to be different.
Wash your hands before you test.
Here’s some of my data. Note that I am not doing more than one fingerstick here. But I find them to be pretty close with this machine.
The %Diff column shows the difference between sensor and manual blood glucose readings. A 20% difference is considered sensor failure.
I am using this machine and a Dexcom G6 sensor. This machine requires a script. It’s not OTC.
Let’s look at a different day.
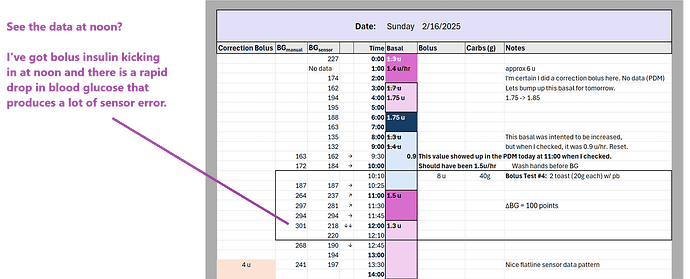
How is the system behaving at noon? Is that a good time to evaluate sensor accuracy?
No, because we see a rapid decrease in BG at noon. See how flaky that sensor data becomes? It is unreliable. The solid circles are manual finger sticks that illustrate a more honest picture of blood glucose during that time interval.
You will always see the sensor become more inaccurate during times of rapid increases and decreases.
You will always see the sensor behave more inaccurately when you are low.
I am producing sensor error all over the place, but that is partially due to the fact that I haven’t adjusted my insulin doses in ages and they are totally wrong. I’m trying to make adjustments quickly in my insulin dosages, so I’m using manual finger sticks to do that, not sensor data.
The sensor data is a mess because I am roller coaster-ing all over the place. Once I make adjustments in my insulin dosing and my BG is more flatline, I can give more credence to sensor readings because a lot of that sensor error falls away naturally once I stop my BG from roller coaster-ing.
My problem in February is rollercoaster-ing from incorrect insulin dosages, not sensor error. If I fix the rollercoaster, then I will fix the sensor error.
By the end of the month, I have fixed that stuff. There’s really no need to look at all those details because system behavior has stabilized.
I can understand where you are coming from, but I don’t share your feelings of frustration. For me, everything is an approximation, and close enough is good enough. That said, I don’t have lax standards.
I build software systems and applications, and by design, they are without error. Still, other systems I deal with are asynchronous, meaning they can run independently and at different times. Occasionally, these differences can lead to inaccuracies, or something flipping back and forth because two systems have differing information. Separately, I work out most days, plus walk 7000+ steps daily. Do I get worried if the system records extra or fewer minutes, or if it miscounts my literal number of steps.
On another level, the absolute number does not matter as much as the trend. I have long used weight scales that incorporate bioimpedance for body fat measurement, and depending on one’s distribution of fat, gender, and fitness, the numbers will vary, but if one measures consistently we can measure the trend, which is more important from a management perspective.
We all have different tolerances for ambiguity, and mine might be a bit higher than most, at least in some domains, but I strive for conciseness in others. My feeling is that you might need to loosen up, if possible, and accept the variation.
Well said. I agree. Trends are important and living a life are important… to much fussing, for me, about numbers, ruins my day.
You reminded me–some years ago when I was first diagnosed and trying to learn just “what was what”–LOL–I felt like the very air I breathed sent my #s up and down more or less randomly! I have stayed away from some technology improvements because I am well known in the family for incidents like absent-mindedly putting the roll of toilet paper in the freezer while deep in a discussion with my sweetie—LOL. I figure that as soon as I get more technologically advanced than a basic meter, I will likely–oh accidentally drop it in the toilet or some such. But I love my old meter. Sturdy as heck and still with me full steam ahead, as they say!..Best to all…Judith
Taking off from what @JamesIgoe said, I think there’s something to be said here about metrology (science of measuring things) and the psychological effect of having these devices put a precise number on something that by its nature isn’t as precise as a single number. When you look at a graph of the results of a scientific experiment, the convention is to put error bars around each point to indicate the range of uncertainty surrounding it. People often say things like “My CGM said 127 but my meter said 131, which one is correct?” The answer is both. Or possibly neither. Both answers may be within the error bars. Do the finger stick again and you’ll rarely get the exact same result. I’ve had two finger sticks be off by 30 or so. You have to consider that the glucose across your whole vascular system at any given moment is going to vary. It’s not going to be perfectly uniform from your toes to the top of your head, or even one hand—or one finger—to the other.
And the tolerances of insulin dosing itself just aren’t that fine.
One of the things in metrology is that different levels of precision are needed for different things. You might need a measurement accurate to a couple angstroms to build your fusion reactor but +/- 1mm is good enough to build your bird house. The whole process of controlling BG through endogenous insulin just isn’t anywhere near as precise as what the level of precision the numbers in our devices imply. It varies by person, of course, but for most of us the difference between a bolus of 4.2 and 4.3 is gonna be totally lost in the noise, even though our pumps make that kind of distinction all the time. You need to have those numbers for carb-counting, but having a number makes us think the whole process has a degree of precision it doesn’t really have. In some ways, the old pre-glucometer method where you match the color of the reagent strip to a swatch on the tube was a more honest representation of what was actually going on.
Great response as usual, Dr BB…There is something to be said for thinking of our numbers in “relative” terms. In what way do our numbers relate to each other given the context of similar circumstances–as an obvious example for a middle aged woman–why the heck am I running so high when everything from time of day to the weather is similar to yesterday when I was in my good range–oh shucks–is it this darn hot flash? Well, one learns that a hot flash will either give you a major spike in your numbers or maybe send you racing to the kitchen and your emergency stash of little tapioca cups to help with a bad low. Both extremes are possible. Such is the nature of diabetes during the whole cycle of menopause…Dear Admin–I’d love to create a safe space for discussions like that. I’m not personally bothered if it involves both our Ladies and our Gentlemen, too. My husband has had to go through it with me, after all! LOL…
I have to agree with @DrBB When I was diagnosed as T2DM 35 years ago I given color changing test strips because us type 2s did not get meters. I use to pass the strip and color chart around the table because it was so flaky.
Then I was prescribed a meter. This was better but the untrained scientist in me would do things like do 2 tests using the same drop of blood. Always diffferent.
The use of a very small drop of blood is never going to be as accurate as a draw of venous blood. There is nearly zero chance of contamination and the sample is much larger. Throughout that sample there will be differences of blood glucose. This gives an average of all those differences which is more accurate that a tiny droplet.
When it comes to CGMs well those do not even measure blood glucose levels but intersitial gluccose levels. When BG is rapidly rising or falling there can be a lag of 15 minutes.
The thing is that there is a margin of error with any self testing. While I would prefer that our metering devices were more accurate, I accept that they are as we use to say in the military, “Close enough for government work,”
Dr BB’s post reminded me of HS Chemistry labs. We would be given different proportions of reagents for a chemical reaction. The results of each team were plotted on a straight line graph.
True confessions time, my group of idiots would know determine eactly what was perfect. We would fudge our results so that our dot was right on the line. Bad boys, Bad. I don’t know why we never got caught when every other team had their results above or below the theoretical perfect line except ours..
CGM measure’s interstitial fluid,not blood like sticking your finger. They are 2 different things.they shouldn’t match.
Nancy50
I use a Dexcom G6; not quite ready to switch to G7. I calibrate using my BG meter. I usually calibrate after putting on a new sensor, then later that day or early the next day. I stop calibrating when the CGM is reasonably close to the meter reading.
I only calibrate when BG level is flat and I have not eaten or exercised recently that would cause it to be trending up or down. Given the BG meter is trying to measure glucose in the blood, and the CGM is measuring glucose in interstitial liquids, and it takes a short while for changes in BG to be reflected in interstitial liquids, it makes sense to calibrate only when BG level is flat.
I re-calibrate whenever the CGM reading does not jibe with how I feel. When the G6 was first released, its initial readings were often significantly different (wrong) from the BG meter readings. Over the last year or so, I have noticed new sensors’ first readings are often much closer to those of the BG meter. But I would never ever trust a sensor that has not been calibrated by my BG meter. Kind of irks me my insurance (Medicare plus a Plan G) will not pay for both my CGM and sufficient test strips to do calibrations. So I pay for the test strips myself.
Having written all that, I am very, very happy with my CGM. It is a game-changer in improving BG management as well as being able to alert me to levels that require my attention. But again, I do not trust my CGM until it has been properly calibrated.
Not sure about the G part but with my Medicaid I told them what they, themselves say that I am entitled to cgms and whatever my pcp writes me separately. At first, getting them to understand the conjunction “AND” used in their instructions means “ BOTH”. Both are correct now and have been for years.
Thanks for that info. I suspect your insurance and mine have different deliberables, but I will look for the language that applies to me and see if I can find something similar.
I can sometimes calibrate a new sensor using just two test strips, but other times it might take 4 or more. After that, I sometimes need to re-calibrate when the CGM reading does not match what I’m feeling.
The last time I looked at the Dexcom instruction manual, it still said to calibrate if the CGM reading did not match what you were feeling, yet Dexcom separately claims (I think starting with G6) that calibration is no longer necessary, and I believe that is why Miedicare refused to pay for test strips. My own experience is that while new sensors now are sometimes acceptably accurate without calibration, I would stop using Dexcom if I were unable to calibrate each new sensor.
Again, thanks for the info. I will follow up.
I change my sensor at bed time. I’ll check that I’m in range before bed and then install new one and go to bed. I’m generally stable over night.
In the morning it’s usually spot on.
That being said, your finger stick meter is also not entirely accurate, so to think of it as a standard might not be the case.
You are calibrating a not so accurate instrument with a different not so accurate instrument.
Luckily for me I can feel when I’m out of range.
I feel low around 60. I feel high around 150.
My cgm is really about adjusting my basal rates so I do t have to pay attention to it. I don’t really expect any home test to be very accurate
Per the G6 manual, fingersticks are required for treatment decisions when symptoms don’t match the reading, calibration is only required if you don’t enter the sensor code or if prompted by the app/reader.
Medicare Part B fixed test strips not being covered when using a CGM in 2023 but did it in a way that makes it unlikely to be useful. Here’s the info Medicare does cover CGM's and Test Strips! ***
Sorry to hear you are struggling to trust your G6. Let us know if you want help with that. Right now my G6 says 77, an hour ago it said 90, I don’t care if the actual number is 67 or 87, I’m going to go have piece of toast.
I never put a sensor in at night, at least not if I can help it! Some of my worst sleepless nights have come from a new sensor going low repeatedly. I much prefer putting it in earlier, and then taking the time to make sure it is stable and calibrated. Even then, a new one sometimes has issues depending on the side I am sleeping on, but that is manageable.
I literally threw away my blood meter, knowing good and well the risks, just so I would have peace of mind as I have scars on all fingers from my obsession. My husband now is borderline diabetic and I’m kicking myself every day for throwing it away. Yes, I could buy a new one but paranoia of buying the best possible one has now plagued me every time I walk into a Wal Mart here in the US.
i actually think it’s good to have more than one, for comparison’s sake. some are more consistent than others, and have different features that you may like better. there’s probably no ‘best possible one’. most today can be trusted i think, but can easily be compared with lab tests.
sorry for typos; i had a stroke 4 weeks ago. most meters are pretty inexpensive, because there’s so much competition, including from CGMs.